Plantar Fasciitis: What You Need to Know
What is Plantar Fasciitis?
Plantar fasciitis is a degenerative condition in which repetitive microtrauma causes a structural breakdown of the connective tissue in the plantar fascia and/or neighboring muscles.
Facts You Need to Know
1 million people receive treatment for this condition annually.
44% of patients with this condition will have pain 15 years after the original diagnosis.
The most common treatment protocols typically used by doctors including: orthotics, corticosteroids, and short-term stretching have NOT been proven to alter long-term outcomes.
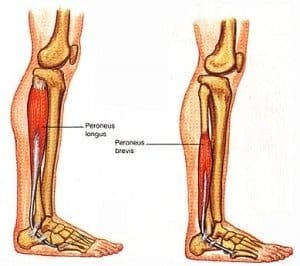
The majority of patients with this condition present with weakness of the peroneal and intrinsic arch muscles, and exercises targeting these muscles mayhems reduce chronicity.
Where to Go From Here
In order to reduce the risk of chronic pain in patient with this condition, we have to follow the new research!
We must: mobilize the restricted joints through the kinetic chain (low back, hips, and ankles), perform soft tissue therapy for any myofascial trigger points throughout the musculature of the legs, and most importantly we must start strengthening the peroneal muscles and the small intrinsic muscles of the feet!
https://www.rslonline.co.uk/news/peroneal-muscles-by-sara-packard/
https://www.physio-pedia.com/index.php?title=File%3A1124_Intrinsic_Muscles_of_the_Foot_b.png&veaction=edit§ion=2
Watch This 2 Minute Video!
We are not your ordinary chiropractic clinic!
Book online today!
Click here to read more information on plantar fasciitis!
Thank you to ChiroUp for providing this information. Research sources are cited below.
1. Riddle D, Schappert S. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: a national study of medical doctors. Foot Ankle Int. 2004;25:303-310.
Hansen L, Krogh T. Ellingson T, et al. Long-term prognosis of plantar fasciitis. A 5- to 15-year follow-up study of 174 patients with ultrasound examination. Orthop J Sportsmed 2018; 6:1-9.
Sullivan J, et al. Musculoskeletal and activity-related factors associated with plantar heel pain. Foot & Ankle Int. 2015; 36:37–45.
Anderson J. Stanek J. Effect of foot orthoses as treatment for plantar fasciitis or heel pain. J Spo Rehab. 2013;22: 130-6.
Protopapas K, Perry S. The effect of a 12-week custom foot orthotic intervention on muscle size and muscle activity of the intrinsic foot muscle of young adults during gait termination. Clinical Biomech. 2020,78.
McClinton S, Collazo C, Vincent E, et al. Impaired foot plantarflexor muscle performance in individuals with plantar heel pain and association with foot orthosis use. J Orthop Sports Phys Ther: 2016;46:681-689.
David J, Sankarapandian V, Christopher P, et al. Injected corticosteroids for treating plantar heel pain in adults. The Cochrane Database of Systematic Reviews. 2017;(6): CD00934
Willwacher S, et al. The potential of toe flexor muscles to enhance performance, Journal of Sports Sciences. 2012;31:424-433.
Song J, Gorelik S, Husang D, Morgan T. Effects of eccentric exercises on foot structure, balance, and dynamic plantar loading. Gait Study Center, Temple University School of Podiatric Medicine. 2019, in press.
DiGiovani C, Kuo R, Tejwani N, et al. Isolated gastrocnemius tightness. J Bone Joint Surg. 2002;(84A):962 971.
Pearce C, Seow D, Lau B. Correlation between gastrocnemius tightness and heel pain severity in plantar fasciitis. Fool Ankle Ini. 2021;42:76-82.
Chimera NJ, Castro M, Manal K. Function and strength following gastrocnemius recession for isolated gastrocnemius contracture. Foot Ankle Ini. 2010:31:377-384.
Arshad Z, Aslam A, Razzaq M, et al. Gastrocnemius release in the management of chronic plantar fasciitis: a systematic review. Foot and Ankle Int. 2021.
Heroux M, Dakin C, Luu B, et al. Absence of lateral gastrocnemius activity and differential motor unit behavior and soleus and medial gastrocnemius during standing balance. J Appl Physiol 2014;116:140-148.
Janda V. Muscle testing and function. Sydney: Butterworths, 1983:230 4.
Panid L, Bogdanis G, Terziz G, et al. Muscle architectural and functional adaptations following 12-weeks of stretching in adolescent female athletes, Frontiers in Physiology. July 2021:12: 701338